How better methadone prescribing has saved more than 2,500 lives
Providing methadone to former heroin addicts can save many lives, if properly done.
But it can also contribute to deaths, if it is consumed in risky ways or diverted to others by those for whom it was intended.
The key to quality assurance is supervised prescribing, as first applied in Scotland and later in England, with dramatic results. In the latest BMJ (1), we have shown that the death rate from methadone in Scotland, which had been 7.0 per 1,000 client-years in 1993-96, fell quickly to 1.0 per 1,000 in 2001-08 after quality assurance was introduced.
As the UK’s coalition government seeks cuts across the board in public spending, the message is that some spending actually saves lives and is cost-effective. So while cuts may be inevitable, they should be planned prudently to spare the spending that earns the best returns.
In England, quality assurance in methadone prescribing took longer to achieve, and the death rate from methadone fell more gradually from 9.9 and 9.0 per 1,000 client-years in 1993-1996 and 1997-2000 to 2.9 and 2.1 per 1,000 client-years in 2001-2004 and 2005-2008 respectively.
What do these figures mean in terms of lives saved? If the death rates achieved in Scotland between 2001 and 2008 had applied in 1993 to 2000, then 36.3 methadone-only drug-related deaths (95% CI: 30.3 to 42.3) would have been expected rather than the 117 observed. Even allowing for random variation, which gives a 97.5 per cent upper bound of 55 on actual deaths, 62 potentially-preventable methadone-only Scottish deaths occurred between 1993 and 2000. Implicitly we are, of course, assuming that heroin overdose fatality would not otherwise have been their inevitable fate.
In 2003, there were 27,400 injecting drug users (2) in Scotland (95 per cent highest probability density interval: 20,700 to 32,100). As methadone provision was then 14,050 client-years (to the nearest 50), then there were roughly twice as many injecting drug users as there were clients receiving methadone.
In England, if the death rate achieved between 2001 and 2008 (2.38 per 1,000 client-years) had applied in 1993-2000, then 356.7 methadone-only deaths would have been expected rather than the 1,406 actually recorded. Allowing for random variation gives an upper bound of 418 on actual deaths so that, conservatively estimated, 988 potentially-preventable methadone-only deaths occurred in England between 1993 and 2000.
There were an estimated 204,000 current injecting drug users in England in 2004/05. England’s methadone provision at that time was 42,500 client-years (to nearest 50), and so those receiving methadone were about one fifth of England’s number of current injectors.
And so our conservative estimate is that some 1,000 methadone-only deaths that might have been prevented occurred in the UK between 1993 and 2000. These deaths are a potent reminder that changes to the manner and quality of methadone prescribing can have beneficial, or lethal, consequences for drug users and others who use methadone that was not prescribed for them.
Methadone-only deaths per 1,000 client-years need to be carefully monitored to ensure that, whether for reasons of political ideology or economy, there is no falling away in the quality of methadone prescribing to vulnerable clients.
Quality-assurance works. We can show that by estimating the numbers of methadone-only deaths that were prevented between 2001 and 2008.
In particular, had Scotland’s 1993-2000 methadone-only death rate applied in 2001-2008, then 454.3 deaths would have been expected (95 per cent CI: 372 to 537) against the 142 actually observed. Conservatively estimated, at the very least, 192 lives were saved during these eight years.
And had England’s 1993-2000 methadone-only death rate applied in 2001-2008, then 3,693 methadone-only DRDs would have been expected (95 per cent CI: 3,500 to 3,767) against the 937 observed. Again, conservatively estimated and with allowance for random variation, at the very least 2,447 lives were saved by quality-assurance in these eight years.
In sum, quality-prescribing of methadone has prevented over 2,600 methadone-only deaths in Scotland and England between 2001 and 2008 and, by smarter implementation, could have prevented 1,000 more in the preceding eight years.
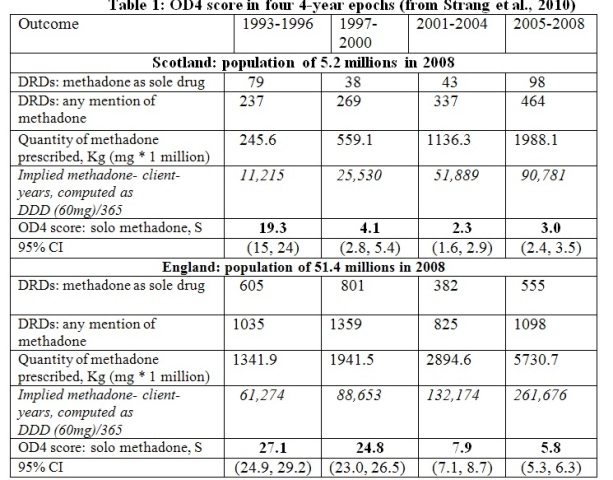
Notes for table 1: OD4 score: solo methadone, S is calculated as follows: DRDs with methadone as sole drug /{quantity of methadone prescribed in Kg /60mg (as daily dose}.
For example, England’s OD4 score of 27.1 in 1993-96 = 605/1341.9 * 60.
In the same period, there were 61,274 implied methadone-client years in England and so methadone-only DRDs occurred at a rate of 605/61.274 = 9.9 per 1,000 client-years in England in 1993-96 (see text).
References
- Strang J, Hall W, Hickman M, Bird SM. The impact of supervised methadone consumption on opiate overdose deaths in England and Scotland. British Medical Journal 2010; 341:638, 640 and online.
- King R, Bird SM, Hay G, Hutchinson SJ. Updated estimation of the prevalence of injecting drug-users in Scotland via capture-recapture methods. Statistical Methods in Medical Research 2009; 18: 341 – 359.



