Where have all the virologists gone?
There are big gaps in UK data on swine flu, many of them because so few virological confirmations of H1N1 seem to be being undertaken anywhere. But virology matters - and if more tests had been done, we might begin to understand why the number of people in hospital for swine flu in England is so much greater than in Scotland.
In the table below, week 31 is defined as midday on Monday 27 July to midday on Monday 3 August, and week 32 as midday on Monday 4 August to midday on Monday 10 August
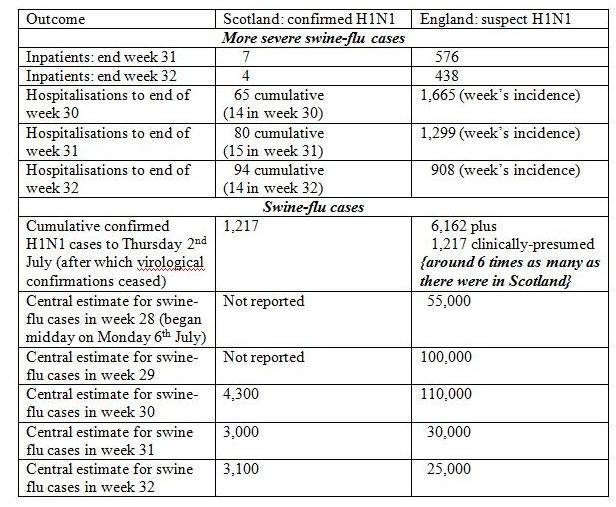
Scotland reported its cumulative incident hospitalisations for confirmed H1N1 up to and including week 31 as 80, with 94 by the end of week 32. As Scotland had admitted 40 confirmed H1N1 cases to hospital by the end of week 27, this suggests a 4-week doubling time for more severe H1N1.
The population of England is 10 times greater than Scotland’s; and swine-flu arrived in England at the same time as in Scotland. For weeks 30, 31 and 32, England had 1,665+1,299 +908 = 3,906 incident hospitalizations for suspect swine-flu, compared with Scotland’s 14 + 15 + 14 = 43 for confirmed H1N1. The number of new hospitalisations for suspect swine-flu in England has been sharply decreasing. But by the end of week 31, while Scotland had seven still-hospitalised patients with confirmed H1N1, England had 576 inpatients with suspected swine-flu. The corresponding figures for the end of week 32 were four in Scotland and 438 in England.
What accounts for these big differences? England has ten times more people than Scotland, but nearly 100 times as many in hospital. Either only one in 10 of those admitted to hospital in England for suspect swine flu actually has the illness, or the H1N1 epidemic has evolved very differently in Scotland and England, in extent and/or timing.
It costs just £27 to test each hospitalised case, using PCR. Is cost deterring virological confirmations? Regional laboratories are tooled up to do such tests. But the recent swine-flu update for week 32 for England provided information neither on the proportion of hospitalised swine-flu cases who had an H1N1 test, nor on their H1N1-confirmation rates by age-group.
Virology is important in an outbreak of infectious disease. Here are six ways in which it matters, and the questions it would answer.
First, by age-group, what proportion of those who consulted their GP about an influenza-like illness in week 33 have swine-flu according to virologists? And what were their swab-compliance rates – how many of those invited to provide a swab for H1N1 confirmation did so?
Second, by age-group, what proportion of those who consulted NHS Direct about an influenza-like illness in week 33 have swine-flu according to virologists? Their swab-compliance rates, number of swabs made available for testing, and sampling scheme for deciding whom (and how many) to ask?
Third, by age-group, what proportion of those who received an authorisation for antiviral medication from the National Pandemic Flu Service (NPFS) in week 33 actually have swine-flu according to virologists? Proportions for NPFS authorizations should surely be considerably higher than those for GP/NHS Direct consultations because authorisation is only agreed to if callers describe symptoms that are those of swine flu.
Fourth, by age-group, what proportion of those admitted to hospital for suspected swine-flu in week 33 have had H1N1 confirmed virologically?
Fifth, by age-group, what proportion of inpatients with suspect swine-flu at the close of week 33 have had their H1N1 confirmed virologically?
More generally, by age-group, what proportion of those who think that they have had swine-flu have H1N1 antibodies? Do they need to be immunized?




Ashley Ford (not verified) wrote,
Thu, 20/08/2009 - 16:12
I agree with your conclusions on the need for sampling, however some of the figures differ from those on the HPA web site for hospitalisations, are there different definitions ?
The HPA say Swine flu hospitalisations in England:
530 patients (hospitalised as of 8am on 05 August)
371 patients (currently hospitalised as of 8am on 12 August)
263 patients (currently hospitalised as of 8am on 19 August).
Anonymous (not verified) wrote,
Thu, 23/12/2010 - 20:17
Hi my son who is 35, contracted swineflu in the hospital he was admitted for something else but he got swineflu, the hospital he was in was Blackpool Victoria hospital they do not swab for swineflu its not their policy they told us, my son had 3 organs failing, we were told he was critical and was dieing, but still they never said it was swineflu it was when he was flown to London brompton and THEY took the swab we found out my son had swineflu and that was why he was dieing,not once did blackpool tell us he had swineflu, we werent gowned or had any masks on neither did the nurses nursing him especially when there was a pandemic we were walking round that hospital mixing with very ill people and we were carrying swineflu on our clothes we even sat in the canteen with many many of the public, this was wrong they kept it quiet, because they didnt want people to know they had swineflu in their hospital my son wasnt even barrier nursed nothing, and now the blackpool victoria hospital is a teaching hospital , why did they not have any infection control for swineflu how did they get away with this, im wondering now because a little 9 year old went in the same hospital with asthma and contracted swineflu as well she was taken to manchester 4 weeks ago but is this week doing well, did they swab this little girl?